Understanding Eating Disorders
Eating disorders are serious mental health conditions characterized by disturbances in eating behaviors and a preoccupation with body weight and shape. These disorders can have significant physical and psychological consequences. In this section, we will explore the definition and overview of eating disorders, as well as their prevalence and impact.
Definition and Overview
Eating disorders encompass a range of conditions, including anorexia nervosa, bulimia nervosa, binge eating disorder, and other specified feeding or eating disorders. Each disorder has its unique set of symptoms and diagnostic criteria, but they all involve a problematic relationship with food and body image.
- Anorexia nervosa: Individuals with anorexia nervosa have an intense fear of gaining weight and a distorted body image. They often restrict their food intake, leading to significant weight loss and physical complications.
- Bulimia nervosa: People with bulimia nervosa typically engage in repeated episodes of binge eating, followed by compensatory behaviors such as self-induced vomiting, excessive exercise, or the use of laxatives. They may also have an excessive focus on body weight and shape.
- Binge eating disorder: This disorder is characterized by recurrent episodes of binge eating, during which individuals consume large quantities of food in a short amount of time while feeling a loss of control. Unlike bulimia nervosa, there are no regular compensatory behaviors.
- Other specified feeding or eating disorders: This category encompasses eating disorders that do not meet the full diagnostic criteria for the above disorders but still involve significant distress and impairment.
Eating disorders can affect individuals of any gender, age, or background. They most commonly develop during adolescence and young adulthood but can occur at any age. It is essential to recognize that eating disorders are not a choice or a lifestyle but rather complex mental illnesses that require professional intervention and support.
Prevalence and Impact
Eating disorders are more prevalent than many people realize. According to the American Psychiatric Association, eating disorders affect up to 5% of the population and have the highest mortality rate of any psychiatric diagnosis other than opioid use disorder. The impact of eating disorders goes beyond physical health concerns, as they can have severe psychological, social, and emotional consequences.
Here are some key statistics regarding specific eating disorders:
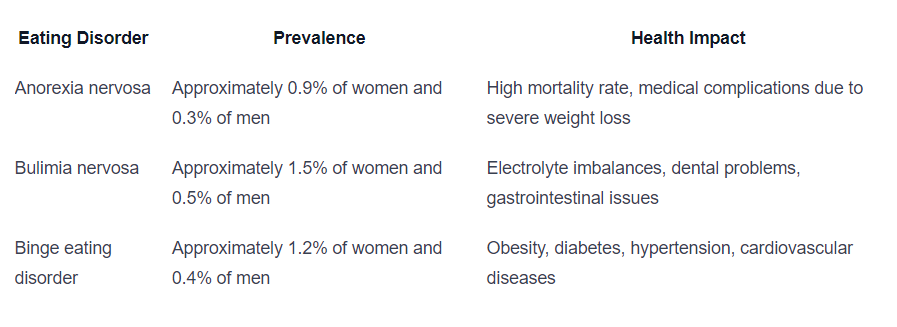
Statistics from the American Psychiatric Association.
It is important to seek early intervention and appropriate treatment for eating disorders to prevent further physical and psychological harm. With proper support, individuals can recover and regain a healthy relationship with food and their bodies.
Autism Spectrum Disorder (ASD) and Eating Disorders
The connection between Autism Spectrum Disorder (ASD) and eating disorders has become an area of interest in research, shedding light on the vulnerabilities and co-occurrence of these conditions. Understanding this relationship is crucial for providing appropriate support and tailored interventions.
Connection and Vulnerabilities
Research suggests that individuals with ASD may be more vulnerable to developing eating disorders. A study found that characteristics specific to ASD contribute to the development of anorexia nervosa, indicating that individuals with ASD may form a vulnerable group for eating disorders.
Moreover, the prevalence of autism spectrum disorder is found to be high in children with anorexia nervosa and avoidant/restrictive food intake disorder. Rates of ASD in these groups were reported to be 16.3% and 12.5%, respectively. These findings highlight the significant co-occurrence of ASD and eating disorders, emphasizing the need for further exploration and understanding.
Research Findings
Studies have delved into the relationship between autistic traits and eating disorders. It has been observed that autistic traits are more common and severe in individuals with anorexia nervosa, as evidenced by higher scores on the Autism Spectrum Quotient Children’s version (AQC) when compared to healthy controls [3]. This suggests a potential link between autistic traits and the development of anorexia nervosa.
In the case of avoidant/restrictive food intake disorder (ARFID), autistic traits are not significantly different from healthy controls. However, correlations exist between AQC and ChEAT26 scores, indicating a potential association between autistic traits and ARFID symptoms. These findings underline the complexity of the relationship between ASD and eating disorders, highlighting the need for further research in this area.
Furthermore, a study exploring the longitudinal relationship between childhood autistic traits and later eating disorder behaviors found that higher levels of childhood autistic traits were associated with a shallower decline in fussy eating between ages 7 and 13. These fussy eating behaviors, in turn, were associated with greater eating disorder behaviors in adolescence. This suggests a potential link between childhood autistic traits and the development of disordered eating later in life.
Understanding the connection between ASD and eating disorders is crucial for developing effective treatment approaches that address the unique needs of individuals with co-occurring conditions. By recognizing the vulnerabilities and considering the research findings, professionals can provide tailored interventions and support to help individuals navigate the challenges associated with both ASD and eating disorders.
Characteristics and Traits
When exploring the co-occurrence of eating disorders and autism, it is important to understand the characteristics and traits that are associated with both conditions. These shared features can provide insight into the complex relationship between autism spectrum disorder (ASD) and eating disorders.
Autistic Traits in Eating Disorders
Research has shown that individuals with eating disorders, such as anorexia nervosa (AN) and avoidant/restrictive food intake disorder (ARFID), often display autistic traits. For example, characteristics specific to ASD were found to contribute to the development of anorexia nervosa. Autistic traits are more common and severe in individuals with AN, as evidenced by higher scores on the Autism Spectrum Quotient Children’s version (AQC) compared to healthy controls.
These shared traits may include difficulties with social interaction, rigid thinking patterns, and sensory sensitivities. Individuals with eating disorders and autism may exhibit challenges in understanding and interpreting social cues, leading to difficulties in forming and maintaining relationships. Additionally, they may struggle with inflexible thinking patterns and have a preference for routine and predictability.
Impact on Symptoms
While autistic traits are not directly linked to the onset and maintenance of eating disorders, they may have an impact on the symptoms experienced by individuals with eating disorders. Autistic traits can exacerbate the severity of eating disorder symptoms, making it more challenging to address and manage these conditions effectively.
In individuals with ARFID, there are significant correlations between total AQC scores (Autism Spectrum Quotient Children’s version) and total Children’s Eating Attitudes Test (ChEAT26) scores, as well as between specific AQC and ChEAT26 subscales This suggests that certain autistic traits may influence the eating attitudes and behaviors exhibited by individuals with ARFID.
Understanding the presence of autistic traits in individuals with eating disorders can help inform treatment approaches and interventions. Tailored strategies that take into account the unique characteristics and needs of individuals with both autism and eating disorders can lead to more effective and comprehensive care. By addressing both conditions simultaneously, healthcare professionals can provide holistic support to individuals navigating the complexities of these co-occurring conditions.
Sensory Factors and Eating Behaviors
Understanding the relationship between sensory factors and eating behaviors is crucial when exploring the co-occurrence of eating disorders and autism. Sensory sensitivities and their impact on food selectivity play a significant role in this context.
Sensory Sensitivities
Sensory sensitivity, such as sensory defensiveness or sensory over-responsivity, may contribute to food selectivity in individuals with autism spectrum disorder (ASD). It is important to note that sensory issues are extremely common in individuals with ASD, with more than 90% of children with ASD having sensory abnormalities and symptoms.
Research suggests that sensory factors such as texture, appearance, taste, smell, and temperature can influence food selectivity in individuals with ASD. The texture of foods is consistently identified as a contributing factor to food acceptance and sensory sensitivity in this population.
Relationship to Food Selectivity
There is consistent evidence of a relationship between sensory processing and a range of eating behaviors in individuals with autism, including taste/smell sensitivities and hypersensitivities. This relationship extends across development.
Sensory processing issues underpin a broad range of eating behaviors in autism, including mealtime behaviors, food selectivity, food refusal, ritualistic eating behaviors, and food neophobia. Taste/smell sensitivities are particularly implicated in the relationship between sensory processing and eating behaviors. Hypersensitivities and the influence of emotions on eating behaviors are also factors that may affect individuals with autism.
To address these challenges, it is important to consider a multidisciplinary approach that incorporates sensory integration techniques, such as desensitization strategies and gradual exposure to different sensory stimuli. Working with professionals who specialize in both autism and eating disorders can help tailor therapeutic strategies to meet the unique needs of individuals with co-occurring conditions.
By understanding the impact of sensory factors on eating behaviors, healthcare professionals can better support individuals with autism and eating disorders. Strategies that address sensory sensitivities and food selectivity can play a crucial role in promoting a healthier relationship with food and overall well-being.
Treatment Approaches
When addressing the co-occurrence of eating disorders and autism, it is essential to implement specific treatment approaches that consider the unique challenges and characteristics of individuals with this comorbidity. Two key approaches in managing this complex combination are addressing comorbidities and employing tailored therapeutic strategies.
Addressing Comorbidities
Treating individuals with the comorbidity of autism and eating disorders requires an integrated approach that acknowledges the interplay between the two conditions. The Maudsley eating disorder team has pioneered a tailored approach to improve and adapt evidence-based treatments for this specific population. The approach aims to address cognitive rigidity, attention to detail, sensory sensitivities, and poor social functioning. By targeting these specific areas, treatment outcomes for patients with this comorbidity can be improved.
Clinicians working with individuals with the comorbidity require additional training to better understand and manage the unique challenges associated with both autism spectrum condition and eating disorders. Training programs can cover topics such as assessment of autism, adaptations in treatment, therapeutic modalities, and sensory adaptations. Evaluation of these training sessions has shown increased clinician confidence in supporting the comorbidity and making necessary adaptations in treatment [7].
Tailored Therapeutic Strategies
Tailoring therapeutic strategies to the specific needs of individuals with the comorbidity of autism and eating disorders is crucial for effective treatment. Environmental adaptations can be made to support individuals, such as creating sensory-friendly ward environments, providing sensory tool kits, and developing specialized menus that address sensory complexities. Occupational therapy and sensory groups can also help individuals explore and address their sensory sensitivities. By reducing sensory overload and creating a more supportive and inclusive treatment environment, these adaptations aim to improve treatment outcomes.
Furthermore, therapeutic strategies should focus on cognitive flexibility, social skills training, and addressing sensory sensitivities. Cognitive-behavioral therapy (CBT) is commonly used in the treatment of eating disorders, and adaptations can be made to incorporate elements that are beneficial for individuals with autism. For instance, incorporating visual supports, structured routines, and social stories can be helpful in improving treatment outcomes for this population.
It is important to note that treatment approaches may vary depending on the severity and individual needs of each person with the comorbidity. Collaborative efforts among clinicians, therapists, and support systems are crucial for a comprehensive and personalized treatment plan. By addressing comorbidities and implementing tailored therapeutic strategies, individuals with the co-occurrence of eating disorders and autism can receive the support and care they need to navigate their recovery journey.
Support and Resources
When it comes to seeking support and resources for individuals dealing with the co-occurrence of eating disorders and autism, there are various options available. These resources aim to provide assistance, guidance, and understanding to both individuals and their families. Some of the key support systems include national helplines and services as well as community awareness initiatives.
National Helplines and Services
One valuable resource for individuals affected by disordered eating and related concerns is the National Eating Disorder Information Centre (NEDIC) in Canada. NEDIC offers a national toll-free helpline and live chat services that provide resources, referrals, and support to individuals across the country. The helpline operates from 9 am to 9 pm Monday to Thursday, 9 am to 5 pm on Friday, and 12 pm to 5 pm on Saturday and Sunday (EST) [8].
NEDIC is committed to supporting individuals who experience eating disorders or disordered eating, regardless of their appearance. They emphasize that bodies do not have to conform to specific standards to be deserving of respect. Their focus is on supporting the individual’s well-being, understanding the impact of their body on how they are perceived and treated [8].
Additionally, NEDIC offers educational materials and resources that specifically address eating disorders within the Black, Indigenous, and People of Colour communities. These resources are created by and for community members and caregivers, aiming to spread awareness and understanding within these groups.
Community Awareness Initiatives
Community awareness initiatives play a vital role in providing support and spreading understanding about eating disorders and autism. These initiatives foster open, supportive dialogue to combat shame, stigma, and silence surrounding these conditions. By acknowledging the presence of nearly 1 million Canadians living with diagnosable eating disorders, they express a commitment to assisting millions more struggling with food and weight preoccupation.
These initiatives aim to create a safe and inclusive space where individuals and their families can find support, share experiences, and access valuable resources. By raising awareness about the co-occurrence of eating disorders and autism, they help to promote understanding and empathy within the community.
In addition to national helplines and services, it is also important to consult with healthcare professionals who specialize in both eating disorders and autism. They can provide tailored guidance and treatment options to address the specific needs of individuals with this comorbidity. The Maudsley eating disorder team, for example, is pioneering a tailored approach to improve and adapt evidence-based treatments for individuals with autism spectrum condition and eating disorder comorbidity. This approach targets cognitive rigidity, attention to detail, sensory sensitivities, and poor social functioning, with the goal of improving treatment outcomes for patients with this co-occurrence.
By utilizing the available national helplines, services, and community awareness initiatives, individuals and their families can find the necessary support and resources to navigate the challenges of eating disorders and autism. These resources aim to provide guidance, understanding, and a sense of community, fostering a path towards healing and well-being.
References
- https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders/
- https://pubmed.ncbi.nlm.nih.gov/32910447/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8130445/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9542277/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601920/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9545673/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7358367/
- https://nedic.ca/

 We've just released an article!
Check out our blog!
We've just released an article!
Check out our blog!